What Actually Causes Osteoarthritis [Part 3: Lifestyle & Inflammation]
Lifestyle.
It’s the factor that seems to be associated with just about every condition people experience in this day and age. But why is that? And how could it possibly be related to osteoarthritis? These are some common questions that get raised by our patients whenever we touch on this point. And today we are here to take our time to finally answer them in detail.
The key that we must first re-iterate from part 1 & 2 is this: Osteoarthritis (OA) is not just a mechanical condition (i.e. wear and tear). The truth is that OA is an inflammatory condition, that is regulated by a whole host of biochemical factors.
if you have been paying attention to our prior posts, you will have noticed just how important exercise is. In Part 1, we showed that the negative effects of ageing can be mitigated by making physical activity a large feature of one’s life. We also showed that exercise will improve all areas of one’s quality of life. Part 2 showcased how strategic exercise and education are both effective tools that can help delay the onset of OA associated with injury. It also showed that a large factor contributing to the progression of OA when an injury takes place is the belief patterns associated and that they can’t be put down to a singular factor.
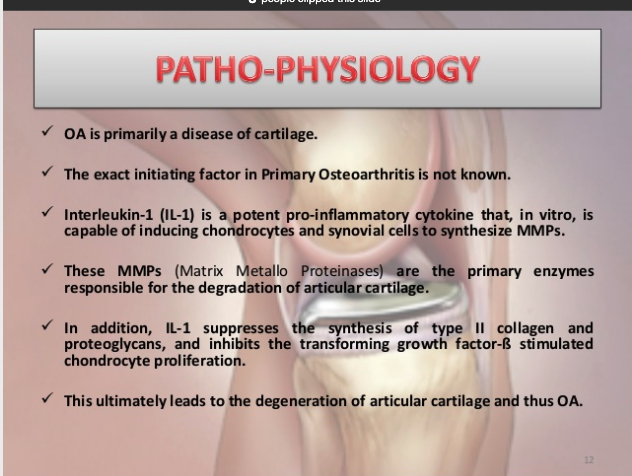
A brief list of some of the biochemical factors that lead to the development of OA, showing that OA is more than just mechanical ‘wear & tear’
And so, with that said we can move onto the 3 factors of lifestyle talked about in part 1 that contribute to worsening outcomes of OA. They are:
- Decreased activity
- Poor dietary choices
- Stress associated Inflammation
Physical Activity
At this point, we have touched on a whole host of factors about the benefits of physical activity and exercise in parts 1 & 2.
Since this article delves into some of the more biochemical factors related to osteoarthritis, we will focus on this component. A recent article highlights some recent research that showed one specific mechanism related to physical activity and mechanical loading of joints, showing that with mechanical loading from physical activity, the body prevented inflammatory chemicals that lead to the degradation of cartilage from being produced. This meant that with increased activity, the body was less likely to produce chemicals that further cause worsening of osteoarthritis.
Similarly, this article shows why physical activity is critical in mitigating the development of osteoarthritis by improving the metabolic status of the body, thus minimising the negative biochemical factors that can contribute to OA.
On the flip side, there can also be negative physical activity, which actually contributes to the worsening and development of OA (see part 5). We see this manifest in people who do too much too soon, or in people who work certain jobs that require awkward physical labour (e.g. frequent bending, twisting, repetitive movement, excess stair climbing). This is known as abnormal joint loading and is an example of physical activity that causes maladaptation (i.e. negative adaptation).
The overall key is that intelligent physical activity is critical to overall health, irrespective of the presence of osteoarthritis. It also shows that osteoarthritis is not simply a condition of ‘wear and tear’, having a whole host of biochemical factors that contribute.
Diet
Firstly, we will talk about diet. There are a number of factors associated with diet that lead to a worsening of OA. However, due to inconclusiveness of the research up to this point, it’s not clear as to which of these specific factors actually cause the OA. All that we know is that with increased body mass beyond a certain point, the effects of OA worsen. Is this due to the 3kg of extra force through the knees for every 1kg of body mass added? Or is it due to the increased inflammatory mediators present in the body in overweight individuals? Or what about the whole host of other factors that have shown to be associated with poor lifestyle? The answer is that we don’t know exactly, but the answer is most likely all of the above. In terms of the weight gain component, we will touch on this in
Because our speciality is in exercise specifically, we would be doing you a disservice to try and answer exactly what dietary factors contribute to OA. We would also be doing you a disservice because the evidence that exists simply isn’t clear enough to say any one particular food, diet or pattern of eating will lead to a worsening or improvement of your osteoarthritis. What we tend to advise is information that falls in line with this generalised guide. The suggestion is to generally follow a balanced, Mediterranean style diet high in fresh fruits & vegetables. This is the perfect example of making sure the basics are taken care of before anything else. For most people, this is a drastic change from what they are currently doing and thus will have huge impacts on their condition. Does this definitely lower the negative effects of inflammation? At present the research is inconclusive, however, the stance we always take is that if it’s in line with the governmental recommendations, then it has merit.
However, what we can say is that there is a strong relationship with overall bodyweight and the symptoms of OA. We will touch on this further in part 4.
Fortunately at MTP Health, we are partnered with a program that addresses this issue of diet and weight loss head-on. The program that we are partnered with, allows patients to get complete access to a comprehensive 18-week program that is aimed to reduce body weight by around 5-10%, hence significantly reducing the risk of OA. It teaches healthy eating habits, while also providing a quick and easy solution for weight loss via meal replacement. This helps patients to see results while learning how to empower themselves to keep the weight off for good. The best part about this program is that it is 100% free for patients involved in participating health funds (feel free to get in touch to see if you may be eligible, our contact details can be found on our site). This program allows us to cover all bases and get some extraordinary results for our patients. While it isn’t the 100% perfect solution for everyone, it is a great option for people who want to take action as quickly and easily as possible. The other alternative we recommend to people is seeing a registered dietician (particularly one that specialises in OA).
Stress Associated Inflammation
Stress is a factor that is often overlooked when we examine the causes of osteoarthritis. This is because there is minimal evidence around ‘stress’ and OA. It is very hard to measure what stress actually means from a research context.
However, what we will be referring to, for the purposes of this article are stressors that cause negative excesses of inflammation. The complete list is far too extensive to list in the confines of this article. There are also certain factors that are only applicable to certain people, as each individual will respond differently to various stimuli. Examples of these negative stressors include: lack of sleep, excess adipose tissue, stressful events, constant sympathetic overdrive, overconsumption of stimulants, lack of rest, dehydration, immune-stimulating foods, alcohol, oxidative factors etc. While the specific factors can be hard to pinpoint, a good rule of thumb is that, if it’s been touted as being ‘unhealthy’ then it may contribute in some way to your condition.
Because we are experts in movement and exercise, we don’t want to get bogged down in this area for too long. We do however want to make mention of this factor, as far too many people fail to consider it’s implications. We regularly see people who have severe OA who live incredibly unhealthy lifestyles and wonder why their condition is getting worse. They often drink barely any water and eat highly processed foods. They work incredibly long hours and stay up late. They are constantly on the go and rarely give themselves a chance to rest.
Remember when we talked about our body being an adaptive organism in part 1? The nature of this means that our body will need time to rest and repair if it is to respond to its stimuli appropriately. If someone is constantly stressed out (causing inflammation) and not giving their body the building blocks it needs to repair, how are they supposed to hope to improve their OA (remember OA is an inflammatory condition)?
Another thing regarding stress and inflammation that we have to touch on is that of the biopsychosocial model of pain. We will touch on this more in part 7. What we want to highlight here is that our beliefs can have a significant impact on our condition. This can also contribute to our stress levels (see HPA axis on the diagram below).
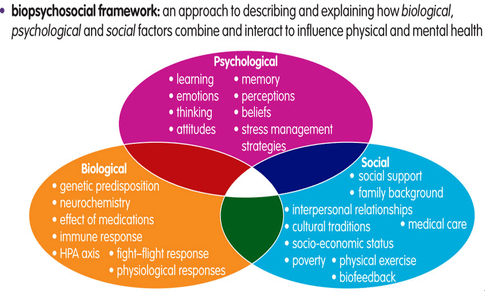
The Biopsychosocial Model and the factors that contribute to pain
While the list of things that cause stress are extensive, the key for our context when looking at OA is that it is often underlooked. Rarely is stress considered when examining a patient.
And this highlights our well-rounded approach to dealing with OA. It showcases that we dig a little deeper than just about everybody else to make sure we address every possible factor, in order to lead to the best result possible.
With all that said, what we typically advise to patients is to clean up the low hanging fruit. They include:
- Sleep: Sleep more. Try to get the recommended 8 hours of sleep (or at l)
- Water: Drink enough water. 8 x 250mL glasses per day is a great start.
- Stimulant regulation: If you think you might be overdoing the stimulants, try to stick to only 1-2 cups of coffee per day.
- Mindful eating: Take your time to eat your food. Constantly eating while in a sympathetic state can impair the ability to digest nutrients. Mindful eating is something that is taught in the 100% free 18-week program that we run with our patients. It can be incredibly useful for weight loss too.
- Weight: Aim for a healthy BMI. Consult your doctor about what would be right for you.
- Diet: Speak with your doctor about the right diet for you. This is something we work with a lot of our patients on.
So there you have it. The next time someone mentions that you might need to clean up your lifestyle, you can now look at some of the factors you might need to address. Our philosophy at MTP Health is that until the most fundamental are factors addressed (i.e. lifestyle), only then should we look to use higher-order interventions.
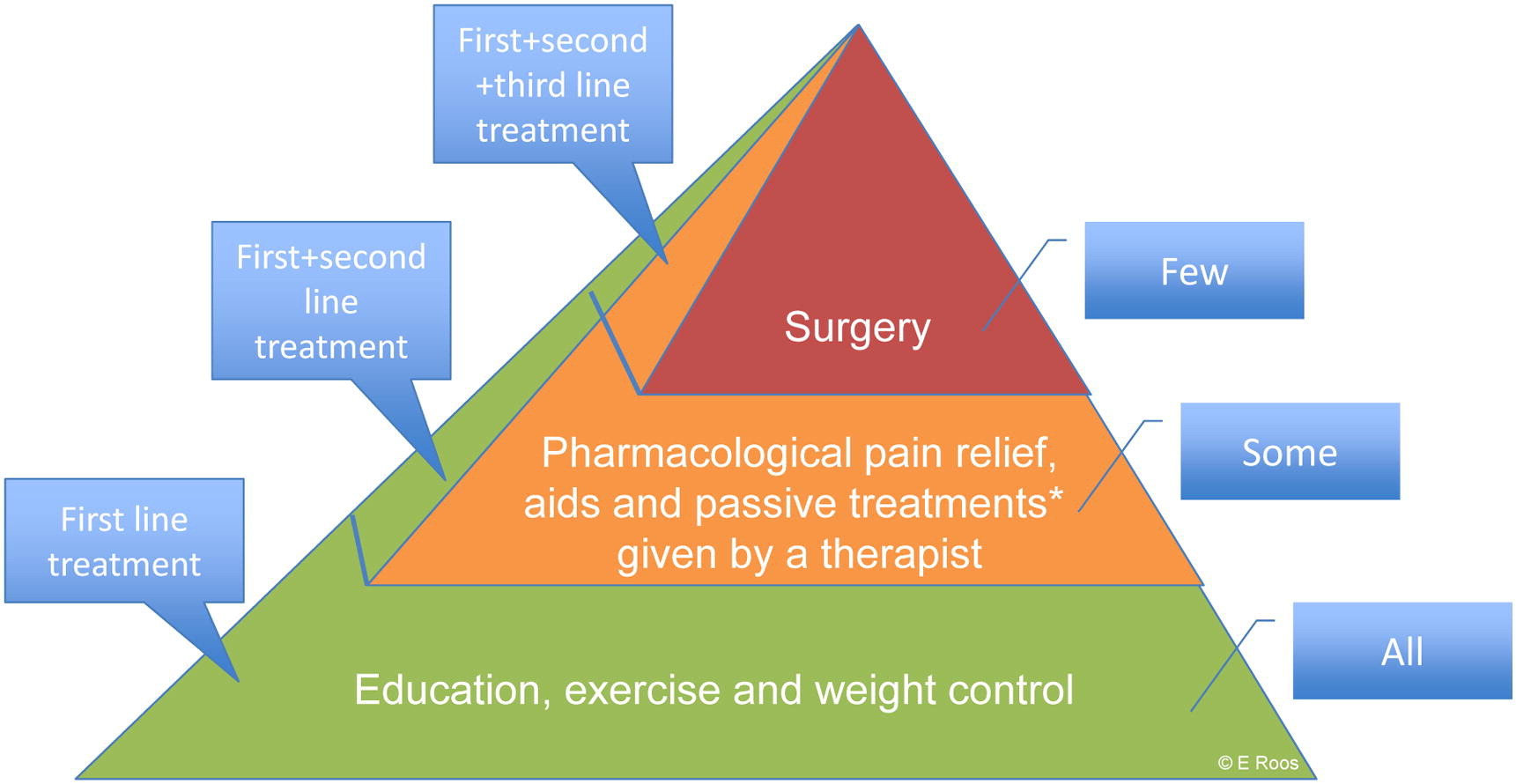
A Pyramid of the Order of Interventions for OA
References
- Exercise helps prevent cartilage damage caused by arthritis
- Osteoarthritis – Why Exercise?
- Occupational and genetic risk factors for osteoarthritis: A review
- Better Health Channel: Osteoarthritis & Diet
- Is There a Dose-Response Relationship Between Weight Loss and Symptom Improvement in Persons With Knee Osteoarthritis?
- Know your brain: The HPA Axis
