What Actually Causes Osteoarthritis [Part 7: Psychology]
The Many Factors At Play When It Comes To Pain
Pain is Simply a Perception of Threat
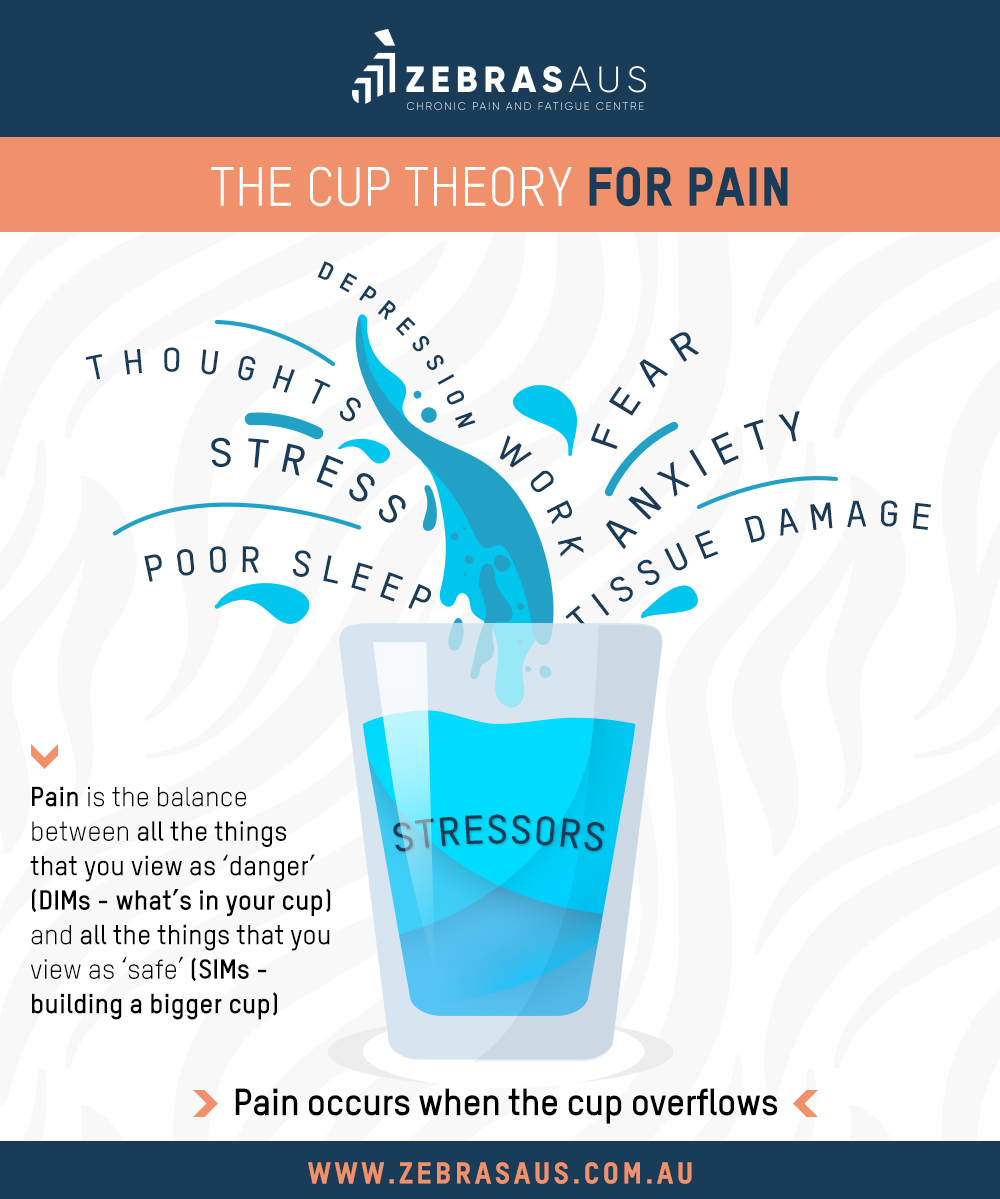
What we instead know to be true, is that pain is simply a gauge of perceived threat. If the body perceives something as dangerous, then it will respond with a painful sensation. We can see this beautifully explained by one of the worlds leading scientists on pain Lorimer Mosely. The problem that arises is when our body perceives threat for a lengthy period of time. This can lead to a re-wiring of the brain, where pain becomes a ‘habit’ of the nervous system. Ever heard the term ‘neurons that fire together, wire together’? Well that’s essentially what can take place if pain becomes a central feature of someones live due to their constant perception of threat and fear of ‘damage’. They may begin to associate pain with certain activities in their life (e.g. Walking up stairs or squatting) and begin completely avoiding that movement. The more they consciously avoid the movement (which is actually impossible, because squatting is a fundamental human movement), the more they reinforce the pain pathway in their brain that tells the body they’re in danger. The creates what is known as a ‘fear avoidant behaviour’ and can lead to drastically worsening pain over time. Eventually, as they begin to experience more and more pain their body will begin to become physically weaker (as we talk about in this article). This is ‘use it or lose it’ in action (see this play out in the example of avoid stairs).
The information outlined above was a bit of a simplification of what actually takes place (for a more comprehensive article read this article), however, it quite nicely illustrates the common story of how pain can become so severe in a lot of the people we see within our daily practice. Essentially all interventions that are used today aim in some way to lower the body’s perception of threat, in order to improve the functional outcomes for the person. There are many ways to skin a cat in this regard, which is why we always like to opt for the safest and least invasive interventions first (i.e. exercise). The beauty of exercise as an intervention is that it does a whole lot for the person more than simply help to minimise their pain. It also has a whole host of other benefits to the person quality of life.
The Key is Education
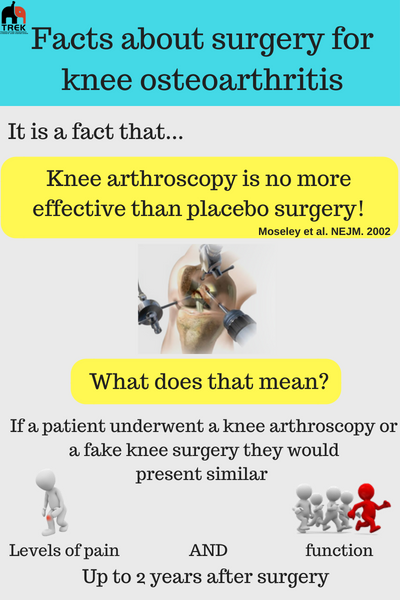
Ultimately though, no intervention is going to be as effective as it could be without a comprehensive education component. If a person doesn’t believe their condition will get better as a result of an intervention, then they won’t. In fact in certain interventions, the placebo effect can account for up to 40% of the result experienced. This can include surgical and pharmaceutical interventions (i.e. drugs and injections). It could also include exercise interventions (this paper shows that changes in pain are not necessarily representative of actual changes in the structure). However, there is still a huge element of the unknown when it comes to the placebo experience. There could very well be a huge number of factors at play that we simply aren’t aware of at this point in time. The key thing to know is that education is an absolutely essential part of improving the experience of a condition such as OA. That’s because evidence is showing that OA does not need to massively impact on someone’s quality of life. This information provides the person with the empowerment they need to take care of their own condition and live their happiest and healthiest life.
An Example of the Effect of Psychology & Perception on the Result that Can be Experienced
And that’s why a large part of what we do and how we view our work is around education.
Education that doesn’t just explain what the condition is, but also addresses common misguided beliefs and myths that exist around a condition. Education that aims to empower by giving the person clear actions that they can begin taking immediately. Education that actually works with the person’s current beliefs and aims to shift them, in order to create a more accurate picture of what their condition actually means + what they can do about it.
All top interventions that deal with osteoarthritis, focus on this education piece as arguably the most critical factor of their success. And the body of evidence completely supports this perspective. So much so that in 2015 and international consensus list of statements for what people with hip & knee OA need to know about their condition was created to more effectively educate all patients with the information they need to empower themselves to manage their condition.
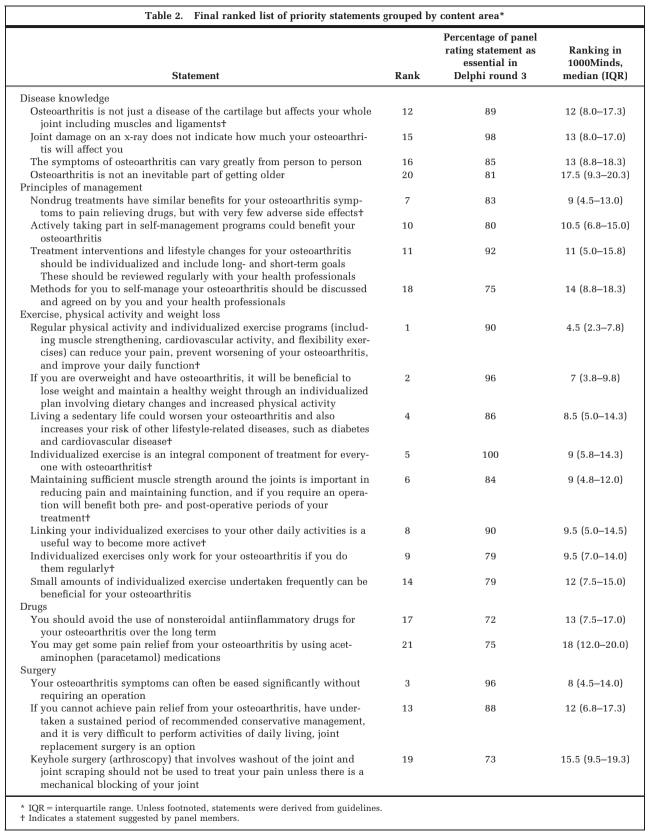
The International List of Education statements for people with Knee & Hip OA
Having a Frame Of Reference
Another incredibly helpful thing for patients who do have OA is to be around other people who suffer from the same condition as them, yet are able to be more functional than they are. A lot of the time people don’t have a frame of reference, thinking that they are the only person who experiences their condition as bad as they do. We see the positive effects this can have on people all the time in our clinic, as patients see people who are able to perform some pretty amazing physical feats, despite their condition. This can have a huge empowering effect for the patient and really helps to highlight all of the information around the perception of threat that we just spoke about above. However, the key is that the person is actually aware of the real story about their pain and genuinely believes that facts that we just outlined. This can be a real struggle for some people who have been experiencing severe pain for a long time. From our experience the key is to be patient and work with the person at their level, handling things with a confident professional tone.
A Close To Home Example
To provide a real-life example of how we see this play out for our patients, we want to share the story of MTP Founder, Luke Kane and his own experience with Knee Pain and OA. Despite having pretty severe damage in one of his knees, Luke has undertaken some pretty amazing physical feats at a world-class level. This example highlights the power that an individuals psychology can have on their experience of their condition and in our eyes is what could be possible for anyone who chooses to not be limited by their condition.
The Biopsychosocial Model
So, now that we’ve touched on how our pain is affected by our beliefs and how crucial education is, we also wanted to re-iterate the biopsychosocial model (see more on this in part 3). This model ties into the image of the cup that we shared above. Essentially what the model outlines is that our pain can be amplified by a whole number of factors in the 3 domains of: biological, psychological & social (see image below for a more comprehensive list). These factors would most commonly be considered ‘stress’ in the way most people describe it. As such with a persons perception of stress and general negative psychology (e.g. anger, frustration, sadness etc.) they can also have a drastic impact on their pain and general overall experience of their condition.
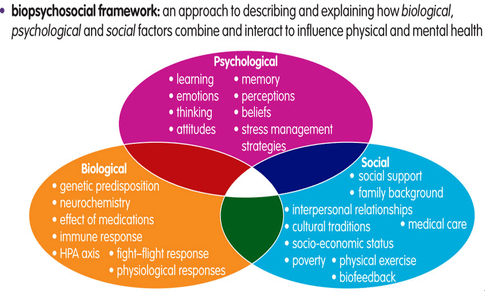
The Biopsychosocial Model and the factors that contribute to pain Pain
Conclusion
So there we have it.
The mind and our psychological state can be the biggest factor that contributes to our Osteoarthritis and experience of our condition. Whether it be through the pain we experience day to day, or the altering of behaviours as a result of our beliefs, there is no doubt that the way we think about our condition will have a drastic impact. The big problem that we have today is that the popular notions that exist don’t necessarily represent the most accurate picture of what OA is all about. As we outlined, while incredibly complex it can have big implications on a persons quality of life.
As such we believe that education aimed at improving someone’s psychology regarding their condition is arguably the most critical component when it comes to improving someone’s experience of OA. This is because we know what is possible when someone does have the right knowledge and frame of mind about their condition. The aim is for the person to choose to not be limited by it. This can be easier said than done, as those who are experiencing the effects of poor psychology will require a lot of re-framing, however, in our experience, the result that is able to be achieved is far worth the effort.
References
- Reconceptualising pain according to modern pain science
- TEDxAdelaide – Lorimer Moseley – Why Things Hurt
- MTP Health: Why You Should Never Avoid Stairs
- Chronic Pain: Where the Body Meets the Brain
- Placebo effects in the pharmacological treatment of uncomplicated benign prostatic hyperplasia. The ALFECH Study Group.
- Placebo-Controlled Trials in Surgery
- Do structural changes (eg, collagen/matrix) explain the response to therapeutic exercises in tendinopathy: a systematic review.
