What is a Baker’s Cyst? How its diagnosed and treated.
Every other day at MTP Health patients present with concerns about being diagnosed with a Baker’s cyst or Popliteal cyst. Understandably, finding out you have a “cyst” in your knee sounds bad. But the good news is they really are harmless. Without a doubt they can be annoying and a little uncomfortable at times but there is no further “damage” occurring due to their existence.
In this blog article we are going to cover the anatomy, diagnosis and treatment options for Baker’s cysts in great detail, because we believe understanding absolutely improves confidence. But before we do, we would like to give an simple analogy for a bakers cyst to help picture what is happening. Imagine for a moment you have a blister on your foot or hand (yes very annoying, but only temporary). The blister is the byproduct of some other aggravation (rubbing or overload incident). The skin responds to the becomes distended as fluid fills under the irritated area. When the irritation settles and the fluid goes you are left with a slightly loose, patch of skin. Now in the case of a bakers cyst, the cyst is the distended pocket of skin that has filled with fluid. It just doesn’t go away like a blister, it stays after the fluid has gone. So next time your knee gets a little aggravated from something the excess fluid fills the loose pocket (cyst) at the back of the knee and feels like you have something blocking the back of the knee. When the irritation settles the fluid goes away and the knee returns to feeling more normal again.
Because the bakers cyst doesn’t go away just fills and empties it is normal to have good and bad times but rest assured it will settle down back to normal and wont be doing any damage in the mean time.
More importantly when it comes to reducing the annoyance of a bakers cyst the aim should be to address whatever is irritating the knee and causing the extra fluid to appear. The cyst filling is just the symptom, address the cause and things will feel better.
Now let’s get into the details.
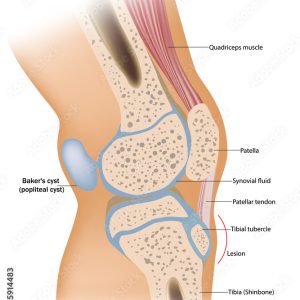
A Baker’s cyst, also known as a popliteal cyst, is a fluid-filled sac that forms behind the knee. They are commonly found in association with intra-articular knee disorders such as osteoarthritis and meniscus tears. The cyst can vary in size where they may be asymptomatic, or can be larger and symptomatic. Baker’s cysts are relatively common, and they can occur in people of all ages. Treatment for a Baker’s cyst can typically involve draining the fluid from the cyst, treating the underlying cause of the cyst in the first place and in some cases surgery may be necessary to remove the cyst.
What are 3 things that increase your risk of developing it?
There are several factors that may increase your risk of developing a Baker’s cyst, including:
- Arthritis: Arthritis is a common cause of Baker’s cysts, particularly osteoarthritis and rheumatoid arthritis.These conditions cause the joint to create excess fluid which can lead to the formation of a cyst.
- Other Knee Conditions: meniscus tears or ACL tears can cause excess fluid in the knee joint, which may increase the risk of developing a Baker’s cyst.
- Age: The risk of developing a Baker’s cyst may be higher in adults, as the risk of developing knee conditions such as arthritis, increases with age.
What are some common signs and symptoms of a Baker’s cyst?
Baker’s cysts can present acutely, or can progress and get worse over time. Some common signs and symptoms of Baker’s cysts are:
- Vague pain behind the knee
- Swelling or a mass at the back of the knee
- Reduced range of motion of the knee. More specifically struggling to bend the knee or hyperextend the knee.
- Tightness behind the knee or stiffness in the back of the knee that can worsen with activity.
While these are common signs and symptoms of a Baker’s Cyst, it is always advised to speak to a healthcare professional to determine the cause of posterior knee pain.

What other medical testing or imaging can be helped with diagnosis?
There are several medical tests and imaging studies that may be used to help diagnose a Baker’s cyst. These may include:
- Ultrasound: Ultrasound uses sound waves to create images of the inside of the body. It can be used to visualise the cyst and the surrounding tissues, as well as to assess the size and shape of the cyst. The advantages of an ultrasound are that it is non-invasive and low radiation. The disadvantages of using an ultrasound as diagnosis of a Baker’s Cyst is that it is difficult to differentiate a popliteal cyst to a meniscal cyst or myxoid tumour.
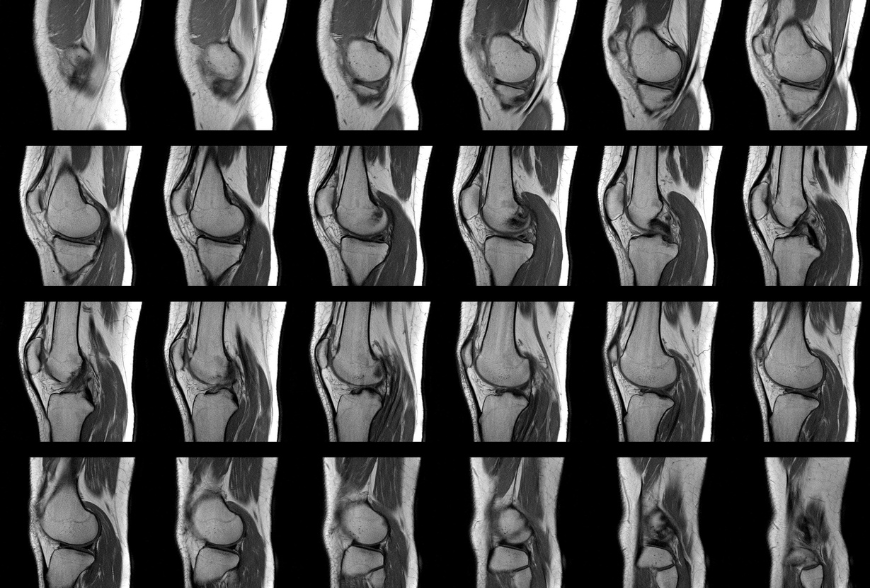
- MRI: An MRI (magnetic resonance imaging) scan uses powerful magnets and radio waves to create detailed images of the inside of the body. An MRI is considered the gold standard for diagnosing a Baker’s Cysts as it looks at the soft tissue abnormalities in the knee as well as having the added advantage of diagnosing other joint pathologies in the knee. The disadvantage of an MRI is that they are expensive, so an ultrasound may be a great option as a screening tool.
- X-ray: An x-ray can help to visualise the bones of the knee joint and can be used to rule out other conditions that may cause similar symptoms, such as a bone tumour or bone fracture.
What are some common differential diagnosis options for Bakers cysts?
There are several conditions that can cause similar symptoms to a Baker’s cyst and may need to be considered as part of the differential diagnosis. These may include:
- Deep vein thrombosis (DVT): This condition occurs when a blood clot forms in the deep veins of the lower leg, and it can cause swelling and pain in the back of the knee. This is a serious condition which a Physiotherapist can assess and refer on if a DVT is suspected.
- Popliteal artery entrapment syndrome: This condition occurs when the popliteal artery, which supplies blood to the lower leg, becomes compressed or trapped, causing pain and swelling in the back of the knee. This condition isn’t common, but again if suspected a Physiotherapist can refer on for further treatment.
- Ligament or tendon injury: An injury to the ligaments or tendons in the knee can cause swelling and pain in the back of the knee. There are a handful of different tendons and ligaments that can be affected in the back of the knee so a thorough assessment would need to be completed in order to appropriately diagnose.
- Calf strain: a tear in the muscle that can involve overstretching or increased load to the calf which can cause pain and swelling into the area. Sometimes these can present quite high in the calf which can also feel as though it is behind the knee. A thorough assessment would need to be performed in order to appropriately diagnose a calf strain.
- Osteoarthritis: This form of arthritis is a degenerative condition that can cause swelling and pain in the knee joint. Further assessment and potentially imaging would need to be done to further diagnose.
- Rheumatoid arthritis: This autoimmune disorder causes inflammation in the joints, including the knee joint, and can cause swelling and pain in the back of the knee.
It is important to note that these are just a few of the conditions that may need to be considered as part of the differential diagnosis, and the specific conditions that are considered may depend on the individual case. It is always advised to seek the advice of a healthcare professional to determine the cause of posterior knee pain.
Is there any evidence for PRP injection, Cortisone injections or Shockwave treatments for this?
There is limited evidence to suggest that PRP injections and shockwave treatments are the most beneficial form of treatment for a Baker’s cyst. PRP injections involve injecting a concentrated solution of platelets, which are a type of cell involved in the healing process, into the affected area. PRP injections are designed to stimulate the healing process and reduce inflammation, however there is limited evidence relating to PRP injections specific to Baker’s cysts.
Shock wave therapy involves the use of high-energy sound waves to stimulate the healing process in the affected area. Again, the evidence suggesting that this is a beneficial option for treating Baker’s cysts is limited and therefore not highly recommended as the first line of treatment.
Cortisone injections are a type of anti-inflammatory medication that can be injected into the affected area to reduce inflammation and pain. Cortisone injections provide short term relief of symptoms of a Baker’s cyst, but do not fix the underlying issue which is eventually what will make your knee symptoms improve. The time that the cortisone injection provides relief is different for each patient and should be advised as to whether this is appropriate for you by your healthcare professional.
It is important to note that these treatments are not universally effective, and the specific treatment that is most appropriate for an individual may depend on the severity of their condition and their overall health. It is also important to note that more research is needed to fully understand the effectiveness and potential risks of these treatments for Baker’s cysts.

What is a typical timeline for recovery from a Baker’s Cyst?
The recovery timeline for a Baker’s cyst can vary depending on the severity of the condition and the treatment that is chosen. The specific recovery timeline will depend on the individual case and the treatment that is chosen. This can vary anywhere from a few weeks to a few months pending the management plan. If the underlying issue is not addressed in the management plan, then the Baker’s cyst will continue to be symptomatic for the patient.
In general, the recovery process may involve the following steps:
- Rest: Initially, it may be necessary to rest the affected leg and avoid activities that cause pain or discomfort.
- Ice: Applying ice to the affected area can help to reduce swelling and inflammation.
- Physiotherapy: In the early stages of management, a physiotherapist can teach you exercises to strengthen the muscles around the knee joint and improve range of motion.
- Medications: Over-the-counter or prescription medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or paracetomol, may be used to reduce inflammation and pain.
- Drainage: If the Baker’s cyst is large or causing significant discomfort, it may be necessary to drain the fluid from the cyst. This can usually be done using a needle and syringe. While draining a cyst, will give you temporary relief, if you do not address the cause of the Bakers cyst in the first place, there is a chance that the Bakers cyst will return.
Can I rupture a Baker’s Cyst myself? If so, is this dangerous?
It is possible to rupture a Baker’s cyst, but it is not common. A Baker’s cyst is a fluid-filled sac that is separated from the joint by a thin wall of tissue. If the cyst becomes very large, the wall of tissue may become stretched and thin, which could potentially lead to the cyst rupturing.
If a Baker’s cyst ruptures, the fluid that is contained within the cyst may leak out into the surrounding tissues such as the calf. This can cause pain and swelling and in rare cases, the fluid from a ruptured Baker’s cyst may enter the bloodstream, which can lead to serious complications such as a DVT.
It is generally not possible to rupture a Baker’s cyst through normal activities, such as walking or moving the leg. However, if the cyst is large and the wall of tissue is thin, it is possible that the cyst could rupture spontaneously. In this case, it is important to seek medical attention as soon as possible
Is there any harm in continuing to exercise/move without specific treatment for a Baker’s Cyst?
If you continue to exercise or move without specific treatment for a Baker’s cyst, it is possible that the cyst could become larger and cause more pain and discomfort. The pressure of the cyst can also cause irritation to surrounding tissues and structures, potentially leading to further injury of those structures. As discussed earlier, in some cases, Baker’s cysts can rupture, causing sudden pain and swelling in the affected area which may affect your ability to exercise.
Furthermore, Baker’s cysts are often associated with other underlying knee conditions such as arthritis, which can worsen over time if left untreated. It is important to address these underlying conditions to prevent long-term damage to the joint. If you have a Baker’s cyst, it is best to consult with a healthcare professional who can provide specific recommendations for treatment and activity modifications to help manage your symptoms and protect your joint health.