Hamstring Tendinosis Part 1 – Diagnosis
If you or someone you know has suffered with lingering or recurrent hamstring or glute pain then this article is for you. Hamstring tendinosis can be a real pain in the butt… So in this 2 part series we are going to take a deep dive into what hamstring tendinosis is, how it is diagnosed, the management strategies we recommend and long term outcomes of hamstring tendinosis rehab.
What is Hamstring Tendinosis?
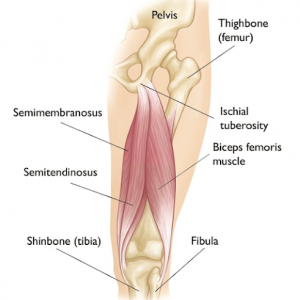
Hamstring Tendinosis is a chronic overload issue of the hamstring resulting in the deterioration of the tendon. This can result in individuals experiencing both pain at rest when sitting (through compression on the tendon), or when active and moving such as walking up stairs or uphill (through increased stretch on the tendon).
Acute muscle injuries of the hamstring i.e. strain or tear, most often occur during high speed running or acute stretch e.g. lunging for a soccer tackle (Mendiguchia et al 2017). The management of proximal hamstring tendinosis is similar to an acute tear or rupture of the proximal hamstring, with a graded loading program based on symptoms, however the recovery time is typically shorter (Goom et al , 2016).
In older adults, the tendon is commonly the weakest point in the muscle – tendon – bone unit due to tendon degeneration or chronic tendinosis, which predisposes the tendon to injury. (Beltran et al, 2012). Due to its chronic nature, hamstring tendinosis can often be a gradual onset of discomfort that is able to be pushed through but gets progressively worse with time. Patients will often report experiencing localised symptoms at the base of the pelvis and often report that symptoms settle after warming up, and then return again after they have cooled down.
Risk Factors for Developing Hamstring Tendinosis:
With every injury there are some associated risk factors that may place you more prone to developing the condition.
- Age:
- This is suggested to be due to loss of strength and poorer load tolerance, however these attributes can be trained!
- Tight hip flexors:
- This can pull the hip into a more tilted position placing increased load on the hamstrings when running and doing sport related activities i.e. kicking (Higashihara 2015).
- Weak supporting muscles:
- Glute med weakness due to increase in hip adduction / pelvic drop during squatting and lunging (Goom 2016)
- Changes in intensity and/or volume of activity:
- Sharp increases in activity is a common trigger for hamstring tendinosis. Things such as big increases in running volume, the introduction of hill runs or sudden increased volume of lunging exercises (Pietrzak 2018)
How is Hamstring Tendinosis Diagnosed?
This is largely dependent on the severity of your presentation but the big 2 are Physio and Imaging.
1. Physiotherapy Assessment:
Just because something hurts doesn’t always mean you have injured that area. Which is why you should always consult your Physiotherapist so they can conduct a thorough history and examination to determine if your pain is irritation to the hamstring tendon or if your pain is secondary and being referred from other areas such as the lumbar spine, sacroiliac joints or the gluteal muscles (Goom et al, 2016).
This diagnostic assessment should typically include (but not limited to):
- Subjective: Background and Patient experience
- History
- Onset and Timeline
- Aggravators & Relievers:
- Patient reported irritants and relievers of symptoms
- Patient expectations:
- Patients own expected recovery time and level of demand tolerance required for full recovery
- History
- Objective: Measurable Function and Tolerance Evaluation
- Stretch:
- Tolerance through range evaluations that place both length and compression demands on the tendon
- Puranen-Orava Test
- Modified Bent Knee Test
- Tolerance through range evaluations that place both length and compression demands on the tendon
- Strength:
- Measuring variation in capacity to express force through the affected side with the non-affected side. This should be done with both isolation and compound movements
- Prone Hip Extension Test
- Prone Knee Flexion Test
- Lunge Test
- Measuring variation in capacity to express force through the affected side with the non-affected side. This should be done with both isolation and compound movements
- Power and Reactive Strength:
- Measuring the tolerance and capacity of under increase dynamic energy and compressive stresses
- Counter-movement Jump Test
- Depth Drop Test
- Measuring the tolerance and capacity of under increase dynamic energy and compressive stresses
- Stretch:
To see demonstration of assessment examples CLICK HERE
If your presentation on assessment is still not clear to your Physio or if your Physio feels there will be added benefit in the information provided by imaging then they will refer you for this.
2. Imaging
An MRI is the primary imaging medium used to identify structural change to the tendon and severity of structural compromise. For instance, if there has been a complete tear otherwise known as ‘avulsion’ from the tendon attachment site, this will be identifiable through MRI. This will assist with ruling in or out other medical intervention beyond exercise rehabilitation alone. However, in the case of tendinosis it is important to note that when undertaking imaging investigation that the degree of change that is evident on the scan does not correlate well with pain scores and that your level of function is a more accurate correlate of pain experience which is great because it is what you can address!
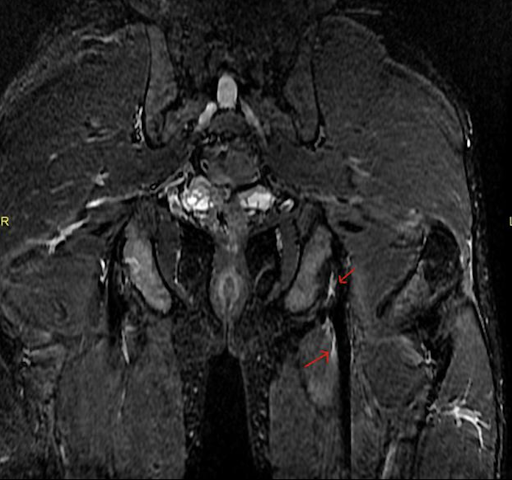
Proximal hamstring avulsion indicated by red arrows.
What to do next?
Through the appropriate assessment with your Physiotherapist a diagnosis can be made, treatment plan established and intervention/treatment can begin.
For more severe cases a referral to a Sports & Exercise Physician might be warranted determine if medical intervention is required prior to commencement of Physiotherapy treatment. In Part 2 of this series we will outline some of the more common medical interventions provided to relieve symptoms.
As you now know the assessment and diagnosis of Hamstring Tendinosis should be layered and comprehensive. There are many factors that need to be considered in this process but once the diagnosis of the injury is made the fundamental objective is to establish your starting point of tolerance of load, stretch and compression so you can take the next, and most important step commencing the rehabilitation.
Remember that the pain you are experiencing is a symptom of your tendon not having the capacity to tolerate the demands of what you are doing. To address this, we need to improve the strength of the tendon & the muscles around the hip and knee!
Read more on breaking the cycle of repeated injuries here
Keep an eye out for our next article on management and recovery!
References
Degen RM. Proximal Hamstring Injuries: Management of Tendinopathy and Avulsion Injuries. Curr Rev Musculoskelet Med. 2019 Jun;12(2):138-146. doi: 10.1007/s12178-019-09541-x. PMID: 30806898; PMCID: PMC6542878.
Goom TS, Malliaras P, Reiman MP, Purdam CR. Proximal Hamstring Tendinopathy: Clinical Aspects of Assessment and Management. J Orthop Sports Phys Ther. 2016 Jun;46(6):483-93. doi: 10.2519/jospt.2016.5986. Epub 2016 Apr 15. PMID: 27084841.
Higashihara A, Nagano Y, Takahashi K, Fukubayashi T. Effects of forward trunk lean on hamstring muscle kinematics during sprinting. J Sports Sci. 2015;33(13):1366-75. doi: 10.1080/02640414.2014.990483. Epub 2014 Dec 16. PMID: 25514378.
Magnusson SP, Langberg H, Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Rev Rheumatol. 2010 May;6(5):262-8. doi: 10.1038/nrrheum.2010.43. Epub 2010 Mar 23. PMID: 20308995.
Mendiguchia, J., Martinez-Ruiz, E., Edouard, P., Morin, J. B., Martinez-Martinez, F., Idoate, F., & Mendez-Villanueva, A. (2017). A Multifactorial, Criteria-based Progressive Algorithm for Hamstring Injury Treatment. Medicine and science in sports and exercise, 49(7), 1482–1492. https://doi.org/10.1249/MSS.0000000000001241
Pietrzak JR, Kayani B, Tahmassebi J, Haddad FS. Proximal hamstring tendinopathy: pathophysiology, diagnosis and treatment. Br J Hosp Med (Lond). 2018 Jul 2;79(7):389-394. doi: 10.12968/hmed.2018.79.7.389. PMID: 29995549.
Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, Cook J. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015 Oct;49(19):1277-83. doi: 10.1136/bjsports-2014-094386. Epub 2015 May 15. PMID: 25979840.
Zissen MH, Wallace G, Stevens KJ, Fredericson M, Beaulieu CF. High hamstring tendinopathy: MRI and ultrasound imaging and therapeutic efficacy of percutaneous corticosteroid injection. AJR Am J Roentgenol. 2010 Oct;195(4):993–998. https://doi. org/10.2214/AJR.09.3674
